A Comprehensive Guide to Weight Loss Procedure
If you’re exploring weight loss options, you might be asking, ‘Is gastric sleeve surgery right for me?’ This definitive guide delves into the critical aspects of sleeve gastrectomy, from understanding the basics of this bariatric procedure, assessing eligibility criteria and the health benefits you can expect, to navigating the recovery process and the risks involved. It’s designed for those seeking clearer insights and preparation for a potentially life-changing decision.
Key Takeaways
- Gastric sleeve surgery, or sleeve gastrectomy, is a popular weight-loss surgery that removes a large portion of the stomach, reducing its size significantly and leading to decreased calorie intake and significant weight loss.
- Candidates for gastric sleeve surgery must have a BMI over 40, or a BMI between 35 and 40 with weight-related health conditions, and are willing to commit to lifestyle changes, with eligibility based on comprehensive medical evaluations.
- Post-surgical care involves a gradual dietary progression, regular medical monitoring, a commitment to diet and exercise changes, and awareness of potential long-term risks such as nutrient deficiencies and food intolerances.
Gastric Sleeve Surgery: An Overview

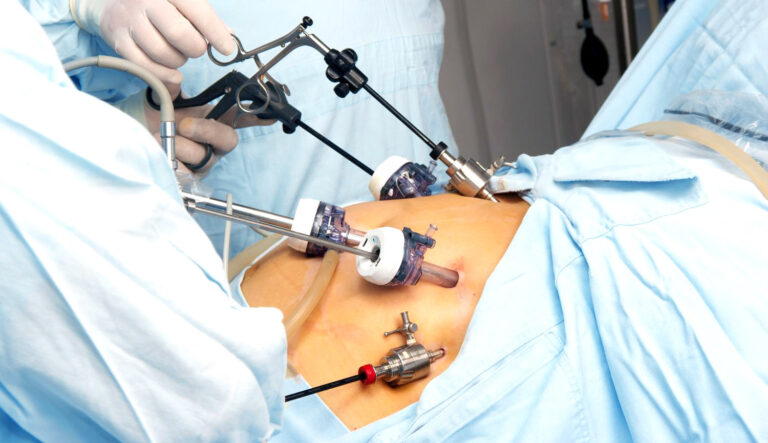
Gastric sleeve surgery, also known as sleeve gastrectomy, is a laparoscopic weight-loss procedure. This method has gained popularity and is now the most commonly performed bariatric surgery in the United States. This surgical procedure involves removing a significant portion of the stomach, leaving behind a narrow, tube-shaped stomach, often likened to the shape of a banana. The result is a reduced capacity for food intake, leading to decreased calorie consumption and, ultimately, weight loss.
This surgery offers benefits that go beyond just weight loss. It can also improve overall health and quality of life. The procedure is known to induce hormonal changes that assist with weight loss and can help relieve conditions associated with being overweight, such as heart disease, high blood pressure, and type 2 diabetes. Gastric sleeve work contributes to these improvements by promoting a healthier lifestyle.
Definition and Procedure
Wondering how this weight loss surgery works? The gastric sleeve procedure involves:
- Removing approximately 80% of the stomach, which results in a smaller, banana-shaped stomach
- Performing the surgical procedure laparoscopically, meaning it involves small incisions in the upper abdomen
- Using a thin, cylindrical tube as a guide to create the new stomach shape, which is then stapled, the excess tissue is removed
The procedure is conducted under general anaesthesia and lasts between one to two hours. The result is a smaller stomach that fills up quicker, leading to a reduced desire to eat and, over time, significant weight loss.
Goals and Benefits
The primary goal of gastric sleeve surgery is, undoubtedly, weight loss. Following surgery, patients can typically anticipate losing up to 60% of their excess body weight within a period of two years. This weight loss can greatly benefit their health and well-being. However, the benefits of this bariatric procedure transcend the scales. For instance, this weight loss surgery has been found to:
- Resolve type 2 diabetes in approximately two-thirds of patients
- Improve the condition in about one-quarter of patients
- Enhance the ability to perform routine daily activities
- Improve overall quality of life
Other benefits include significant weight loss without rerouting of the intestines and potentially shorter hospital stays compared to other surgical procedures.
Determining Eligibility for Gastric Sleeve Surgery

Although gastric sleeve surgery might appear as an appealing option, it’s worth noting that it’s not a viable solution for everyone. The procedure is designed for individuals with a BMI over 40 or those with a BMI between 35 and 40 accompanied by obesity-related health conditions such as sleep apnea, high blood pressure, heart disease, or type 2 diabetes. Furthermore, it’s typically recommended for those who have a history of unsuccessful long-term weight loss through other methods.
However, eligibility is not strictly confined to these parameters. For patients with a higher BMI (such as over 50) or severe health issues like GERD or those on insulin for diabetes, gastric bypass might be a more appropriate procedure. This suggests that gastric sleeve surgery could be recommended for patients without these specific conditions.
Medical Guidelines
The medical guidelines for eligibility for gastric sleeve surgery are quite specific. A patient may qualify for sleeve gastrectomy surgery if they meet one of the following criteria:
- BMI of 40 or higher
- BMI of 35 to 39.9 and suffer from a serious weight-related health issue
- BMI of 30 to 35 when accompanied by uncontrollable diabetes or metabolic syndrome
- BMI between 35 and 40 with major health complications like diabetes or cardiovascular disease
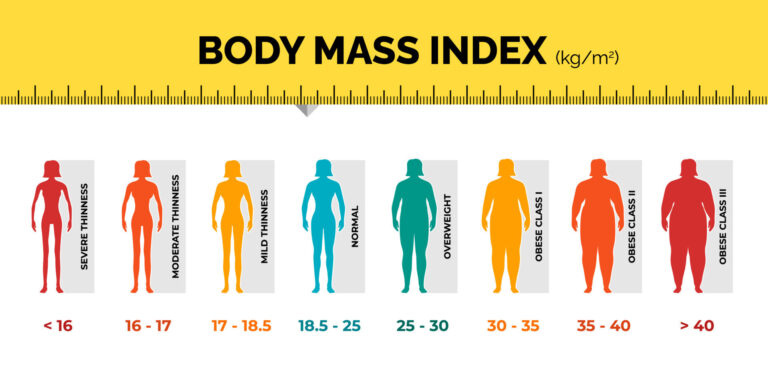
You can calculate your BMI using a free calculator Here.
However, medical conditions are not the only factors considered in bariatric surgery. There must be no evidence of active alcoholism, drug addiction, or major psychiatric disorders for a patient to be eligible for surgery.
Additional factors, such as the patient’s age and general health, including the presence of heart or lung diseases, are also taken into account to determine the appropriateness of bariatric surgery.
Lifestyle Changes and Commitment
Beyond medical guidelines, lifestyle changes and commitment play a crucial role in determining eligibility for gastric sleeve surgery. Candidates must:
- Be willing to make permanent lifestyle changes
- Commit to post-surgery follow-ups
- Have a documented history of weight management and previous weight loss attempts with supervised diets and exercise
These requirements may also be necessary for insurance coverage.
Psychological evaluations are often conducted to assess a patient’s understanding of the surgery’s risks and their commitment to adhere to the recovery plans. The post-surgery period may present psychological challenges, and patients are encouraged to communicate any difficulties to their doctor.
Preparing for Gastric Sleeve Surgery

Upon establishing eligibility, the preparation phase for surgery begins. The process entails several pre-operative requirements, including losing a certain amount of weight and participating in counselling or physical therapy sessions. As part of the pre-operative preparations, it’s strongly advised that candidates stop smoking at least 4 to 6 weeks prior to the surgery to lower surgical and postoperative risks.
Before undergoing gastric sleeve surgery, the patient must complete pre-surgery tests and evaluations, which are vital to establishing their readiness for the procedure. During the pre-surgery consultation, patients are expected to bring important documentation, including:
- A diet history
- Reports from special tests conducted
- Hospital discharge summaries
- A comprehensive list of any medications they’re currently taking.
Pre-Surgery Tests and Evaluations
Pre-surgery tests for bariatric surgery candidates typically include a Complete Blood Count (CBC), Urinalysis, a Chemistry Panel, a chest X-ray, and an electrocardiogram. However, additional evaluations such as a gallbladder ultrasound, pulmonary function testing, echocardiogram, sleep studies, GI evaluation, cardiology evaluation, or psychiatric evaluation may be requested based on individual health needs.
Candidates undergo pre-operative medical and surgical screening to ensure they are healthy enough for bariatric surgery and to determine if there are obesity-related diseases affecting their health. A comprehensive evaluation includes nutritional assessment, possibly physical therapy, and social service evaluations, to identify any medical issues that may preclude patients from bariatric surgery procedures.
Psychological evaluations are conducted to assess the patient’s psychiatric history, current psychological function, weight and dieting history, eating behaviours, and physical activity.
Diet and Exercise Modifications
Alongside these evaluations, specific dietary changes are also necessary before bariatric surgery. These changes, which include reducing calorie and carbohydrate intake and increasing healthy fats, are crucial for the safety of the surgery. They help reduce the size of the liver and the amount of fat around the stomach. A high-protein, low-calorie diet is recommended to preserve muscle tissue, necessitating an intake of about 60–80 grams of protein per day.
In addition to dietary changes, establishing an exercise routine before surgery is equally important. Activities such as low-impact aerobics, strength training, and yoga can improve the candidate’s physical fitness, reduce surgical risk, and aid long-term weight management after surgery.
Recovery and Post-Surgery Care

Following the gastric sleeve surgery, the path to recovery commences. This period involves frequent medical check-ups, laboratory testing, blood work, and various exams to monitor the patient’s recovery. Additionally, a gradual dietary progression is necessary, moving from a liquid diet to pureed and soft foods, and eventually to regular foods as part of the recovery process.
Post-surgery care also includes changes in diet and the introduction of exercise. Initially, this starts with walking a few minutes each day and escalates to more extensive exercise regimens about six weeks after surgery. It’s important to note that weight loss expectations post-surgery are variable, with no set standard for the amount lost in the first few years, making adherence to a diet and exercise plan crucial for maximizing surgery results.
Diet Progression
The progression of the diet post-surgery is a gradual process. For the first two weeks after bariatric surgery, a liquid diet is implemented to avoid putting pressure on the healing wounds and to adjust to the new stomach size. In weeks three and four post-surgery, patients transition to a pureed food diet, which consists of smooth foods with no lumps, starting from 2-3 tablespoons to 4-6 tablespoons per meal.
From weeks five to eight, a soft diet is introduced, with foods that can fall apart easily. After eight weeks, a balanced diet low in fat and sugar, focusing on lean protein and fibre, is recommended to establish healthy eating habits.
Ongoing Monitoring and Support
Regular follow-up appointments after weight-loss surgery are vital for monitoring progress and preventing weight gain. These appointments become less frequent after the first year but remain crucial for long-term weight loss success.
Additionally, after surgery, it is important to:
- Have regular blood tests to monitor for potential nutritional deficiencies
- Take a daily multivitamin and calcium-vitamin D supplements
- Seek psychological support for mental health and relationship issues
- Be aware of the possibility of addiction transferring to substances or behaviors other than overeating
Comparing Gastric Sleeve Surgery to Other Bariatric Procedures
Although gastric sleeve surgery has demonstrated effectiveness for many patients, it’s among several weight loss procedures (bariatric surgery) accessible today. It’s simpler than other bariatric surgeries and involves fewer changes to the patient’s overall anatomy compared to gastric bypass surgery, which creates a small stomach pouch connected to the small intestine.
Alternatively, laparoscopic adjustable gastric banding involves placing a silicone band around the upper part of the stomach to control its size, different from the permanent removal of a stomach portion in gastric sleeve surgery. Despite these differences, gastric sleeve surgery can lead to about 60% excess weight loss within the first two years, which is nearly as effective as gastric bypass surgery.
Gastric Bypass Surgery
Gastric bypass surgery, another commonly performed weight loss procedure, has a unique set of considerations. It involves creating a small stomach pouch connected to the small intestine, which can potentially lead to more significant weight loss compared to a gastric sleeve. However, it may cause dumping syndrome, a condition characterized by abdominal pain, cramping, nausea, weakness, sweating, faintness, and diarrhoea after eating due to the rapid passage of food into the small intestine.
While the potential for greater weight loss may make gastric bypass surgery an attractive choice for some, the prospect of dealing with dumping syndrome and the more complex nature of the procedure are factors to consider when choosing a weight loss procedure.
Laparoscopic Adjustable Gastric Banding
As another alternative in bariatric surgery, laparoscopic adjustable gastric banding is less invasive and has a lower risk of complications compared to gastric sleeve surgery. However, it may lead to less weight loss and require more long-term adjustments.
Unlike gastric sleeve surgery, laparoscopic adjustable gastric banding does not involve cutting or removing stomach tissue. Instead, a silicone band is placed around the upper part of the stomach, providing the following benefits:
- The option for the band to be adjusted or removed if needed
- Less invasive procedure compared to gastric sleeve
- Potential for weight loss and improved health without permanent changes to the stomach
This makes laparoscopic adjustable gastric banding, a form of laparoscopic surgery, a popular choice for individuals seeking a reversible weight loss solution.
Potential Risks and Complications
As with any surgical process, the gastric sleeve carries potential risks and complications. These vary depending on the type of surgery and can include leakage, strictures, and worsening reflux.
Common risks include infections at the surgical site and complications related to tobacco use. Patients are strongly advised to cease smoking at least 4 to 6 weeks prior to the surgery to lower surgical and postoperative risks.
Common Risks
Infections at the surgical site represent a common postoperative complication that requires immediate attention to prevent further issues. This is why it’s important to follow post-surgery care instructions closely and maintain regular follow-up appointments with the surgical team.
Tobacco use also compounds surgical risks, making smoking cessation crucial before surgery. The harmful effects of smoking can interfere with the healing process and increase the risk of complications.
Long-Term Complications
Long-term complications can also arise following a gastric sleeve operation. Nutrient deficiencies, especially in zinc, calcium, and vitamin D, are common after bariatric surgery. This can sometimes lead to conditions such as osteoporosis and necessitate supplements.
Other complications that may present over time include:
- Food intolerances
- Hypoglycemia
- Gallstone formation potentially requires gallbladder removal
- Incisional hernias manifest as bulges at the incision site.
How to Deal with Weight Loss, Regain, and Plateaus

A plateau occurs when the caloric expenditure equals the caloric intake. To accomplish higher weight loss, either increase your degree of physical activity or cut your caloric consumption.
Even with the established efficacy of gastric sleeve surgery, patients may occasionally encounter plateaus in weight loss plateaus and regain. Weight loss plateaus often occur around 3 to 6 months post-surgery, and weight regain is typically observed starting in the third year, primarily affected by dietary habits and sleeve size.
To overcome weight loss plateaus and prevent weight gain after bariatric surgery, it’s essential for patients looking to lose weight to:
- Maintain a healthy diet
- Engage in regular physical activity
- Prioritize sleep
- Manage stress
- Consider taking regular body measurements
Following these steps makes losing weight a more achievable and sustainable goal.
These strategies can help overcome plateaus by providing a more comprehensive view of body changes, including body mass index, beyond the scale.
Support groups can also be beneficial to help patients cope with psychological or emotional challenges post-surgery, aiding in the continuation of weight loss efforts and in dealing with times of weight plateaus and regain.
Summary
Throughout this comprehensive guide, we’ve explored gastric sleeve surgery in-depth, understanding its procedure, benefits, eligibility criteria, and potential risks. We’ve also looked at how it compares to other weight loss procedures and how to manage common post-surgery challenges like weight loss plateaus and regain.
Gastric sleeve surgery offers a potentially transformative path for those struggling with weight loss. However, it’s important to remember that it’s not a magic bullet, but rather a tool that can aid in weight loss when combined with lifestyle changes and ongoing support. If you’re considering gastric sleeve surgery as a bariatric surgery, consult a healthcare professional to discuss your options and determine the best course of action for your health journey.
Frequently Asked Questions
What are the downsides of the gastric sleeve?
The downsides of gastric sleeve operations include potential long-term complications such as gastrointestinal obstruction, hernias, reflux, hypoglycemia, malnutrition, and vomiting. It’s important to discuss these risks with your doctor before considering the procedure.
Are gastric sleeves worth it?
Yes, gastric sleeves are worth it because they offer excellent weight loss and health benefits without causing long-term complications related to nutrition.
How painful is gastric sleeve surgery?
Gastric sleeve surgery is generally not very painful during and immediately after the procedure due to the effects of anaesthesia and pain medications. However, some discomfort is to be expected in the following days as the anaesthesia wears off and mobility increases.
How does the gastric sleeve work?
The gastric sleeve works by removing a large portion of the stomach, leaving behind a narrow tube called a sleeve. After the surgery, food still travels from the stomach to the small intestine.
What is gastric sleeve surgery?
Gastric sleeve surgery, also known as sleeve gastrectomy, involves removing a significant portion of the stomach to create a narrow, tube-shaped stomach, promoting weight loss.


Test Comment
This is a reply
Another comment